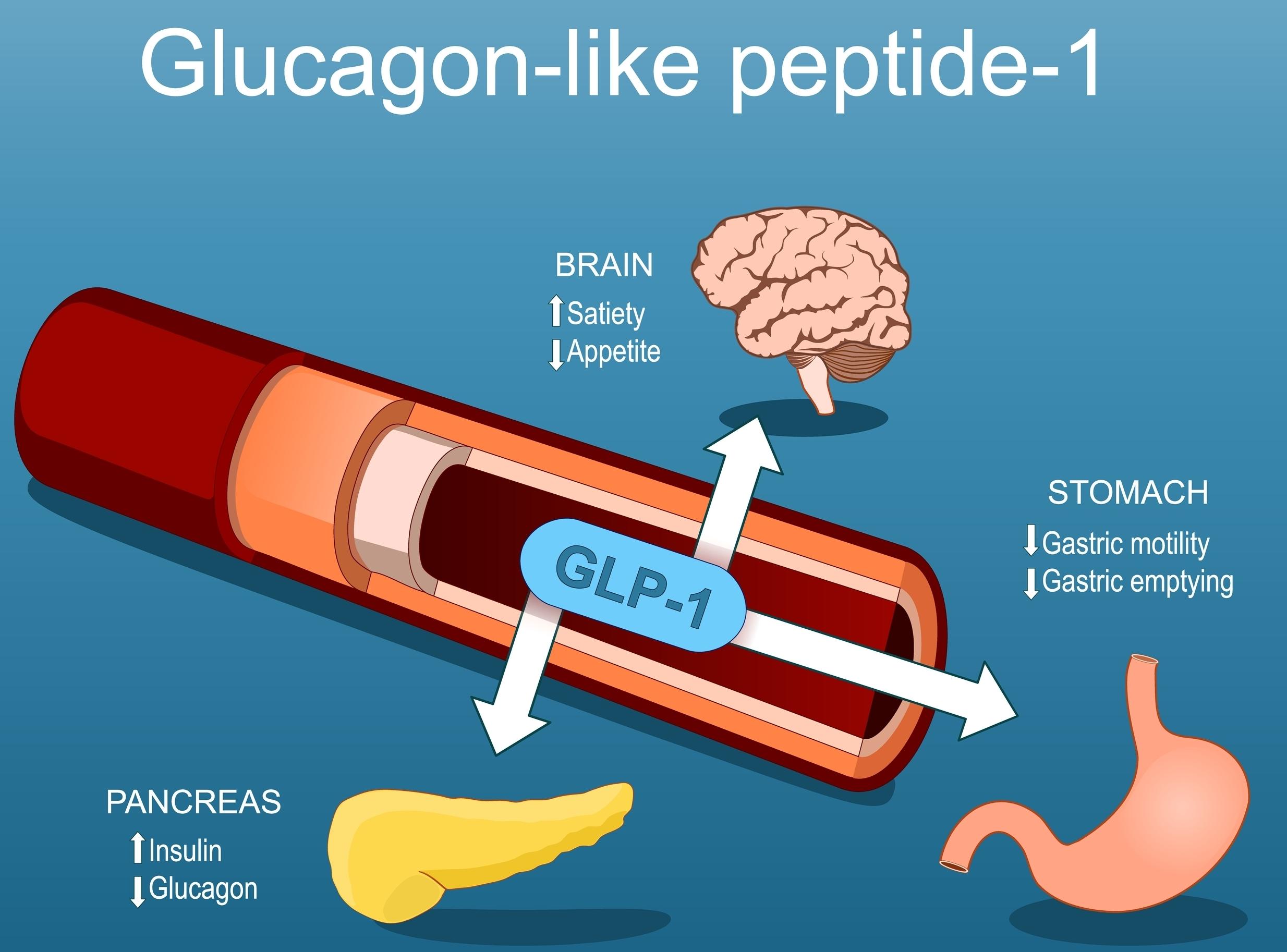
Glucagon-like peptide-1 (GLP-1) is an incretin hormone secreted by intestinal L cells in response to dietary intake. Within minutes after a meal, GLP-1 is released from the L cells in the ileum and colon and regulates insulin secretion in a glucose-dependent manner. When GLP-1 reaches the pancreas, it binds to the GLP-1 receptors (GLP-1R) expressed on pancreatic β cells, stimulating insulin release. Because this action is directly related to blood glucose levels, it can reduce the risk of hypoglycemia. Additionally, GLP-1 promotes the growth and proliferation of pancreatic β cells, inhibits glucagon secretion, and enhances peripheral tissue uptake of glucose, making it a key factor in maintaining stable blood glucose levels.
However, the half-life of natural GLP-1 is very short, lasting only 1-2 minutes in the bloodstream. Extending its duration of action has become a focus of drug development. As a result, GLP-1 receptor agonists (GLP-1RAs) have been developed. These are analogs of GLP-1 with longer half-lives and sustained action, effectively enhancing insulin secretion and inhibiting glucagon release. GLP-1RAs are widely used for the treatment of type 2 diabetes mellitus (T2DM).
Research indicates that GLP-1 receptors are present in multiple organs, including the pancreas, heart, and kidneys, suggesting that GLP-1RAs have a broad range of pharmacological effects. In addition to lowering blood glucose levels, GLP-1RAs can increase satiety, promote weight loss, and offer potential cardiovascular protection. Moreover, GLP-1 and its analogs have shown positive effects in renal protection, neuroprotection, and lipid metabolism regulation, with promising prospects for treating conditions such as non-alcoholic steatohepatitis (NASH) and Alzheimer’s disease.
FDA approved GLP-1 receptor agonists for type 2 diabetes mellitus

GLP-1 receptor agonists at BOC Sciences
Future trends in the development of GLP-1 receptor agonists
Looking back at the development of GLP-1 receptor agonists (GLP-1 RAs), two main goals have consistently guided their advancement: improving patient compliance and enhancing product efficacy. However, with increasing competition in the GLP-1 RA market, merely relying on efficacy is no longer sufficient for a product to stand out. In the future, innovation may focus on five key areas: long-acting formulations, oral delivery methods, multi-target combination therapies, and expanding the range of indications.
Long-acting formulations
GLP-1 RAs can be categorized into two main types: short-acting and long-acting. Short-acting drugs primarily lower postprandial blood glucose levels by slowing gastric emptying, while long-acting GLP-1 RAs are more effective at reducing fasting blood glucose levels, mainly by promoting insulin secretion and inhibiting glucagon release. Both types of medications effectively lower blood glucose, but long-acting drugs may dominate the market due to higher patient compliance. Common strategies to extend the duration of GLP-1 RAs include:
Amino Acid Sequence Optimization: Reducing rapid degradation by DPP-4 enzymes to prolong the drug’s half-life.
Fusion Proteins: Utilizing fusion proteins such as albumin or Fc fragments to increase the molecular weight of the drug, reducing rapid renal filtration and coordinating with other mechanisms to extend in vivo circulation time.
Fatty Acid Modifications: Exploiting the interactions between fatty acids and albumin to achieve metabolic stability and circulation, while using the self-assembly and ionic properties of fatty acids to prolong the drug’s half-life.
PEGylation: Increasing the molecular size of the drug to slow enzymatic degradation.
Polymer-Based Sustained Release Formulations: Developing sustained release formulations to extend the release time of the drug in the body.
Oral Formulations
The only available oral GLP-1 receptor agonist is semaglutide (Rybelsus, Novo Nordisk). Its oral bioavailability is achieved through the incorporation of the absorption enhancer SNAC (N-[8-(2-hydroxybenzoyl)amino]octanoic acid), which works through two mechanisms: (1) temporarily raising the local pH in the stomach to reduce gastric protease activity; and (2) forming hydrophobic ion pairs (HIP) with the peptide drug to enhance its membrane permeability. This approach significantly improves the bioavailability of the oral medication.
The advantages of oral peptide GLP-1 RAs include high efficacy, low dosage requirements, and low toxicity. The molecular size of peptides lies between that of small molecule drugs and large protein drugs, providing higher activity and better selectivity compared to small molecule drugs.
However, these medications also face several challenges, including low stability in the body, short half-lives, poor membrane permeability, complex manufacturing processes, and high costs. Additionally, the administration of oral GLP-1 drugs requires strict guidance: for example, semaglutide must be taken on an empty stomach in the morning, with no more than 120 mL of water, and patients must wait at least 30 minutes before having breakfast.
Multi-Target Synergistic Effects
GLP-1 receptors (GLP-1R) play a key role in regulating glucose balance, fat metabolism, and food intake. Additionally, the glucagon receptor (GCGR), glucose-dependent insulinotropic polypeptide receptor (GIPR), and fibroblast growth factor 21 receptor (FG21R) significantly impact these metabolic processes. GLP-1R, GIPR, and GCGR are all present in pancreatic β cells. Activation of these receptors during glucose regulation helps improve β-cell function and protect the pancreas, enhancing insulin secretion and better controlling blood glucose levels. Tirzepatide, developed by Eli Lilly, is the world’s first dual GLP-1R/GIPR agonist and has shown superior weight loss effects compared to semaglutide.
In addition to dual GLP-1R/GIPR-targeted drugs, the development of GLP-1R/GCGR dual-target drugs and GLP-1R/GIPR/GCGR triple-target drugs is a focus of ongoing multi-target GLP-1 drug development. Several drugs are currently in advanced clinical trials:
Phase III Clinical Trials: IBI362 (Innovent/Eli Lilly), CagriSema (Novo Nordisk), Retatrutide (Eli Lilly), and Survodutide (Boehringer Ingelheim).
Phase II Clinical Trials: Efinopegdutide (Merck/Johnson & Johnson/Hanmi Hanma), VK2735 (Viking Therapeutics), BGM0504 (BrightGene), Pemvidutide (Altimmune/Spitfire Pharma), AMG133 (Amgen), Dapiglutide (Zealand Pharma), etc.
Combination therapies and expanding indications
Combination therapy often results in synergistic effects, with benefits that surpass the sum of individual treatments. Using GLP-1 RAs in conjunction with other glucose-lowering or cardiovascular medications can significantly enhance treatment effectiveness, reduce side effects, and better meet the diverse needs of different patients. For instance, Novo Nordisk’s CagriSema, a combination of semaglutide and cagrilintide, has shown superior results in lowering blood glucose and promoting weight loss compared to semaglutide alone.
Moreover, expanding indications aims to explore new markets. GLP-1 RAs are currently being investigated for various new areas, such as cardiovascular diseases, non-alcoholic steatohepatitis (NASH), Alzheimer’s disease, and chronic kidney disease. These new indications could present growth opportunities for GLP-1 drugs and offer broader treatment options for more patients.
Conclusion
The GLP-1 drug market is rapidly expanding, driving strong enthusiasm among companies for the development of GLP-1 medications. In recent years, the number of drug pipelines has steadily increased. Looking ahead, with breakthroughs in novel molecular designs, oral formulations, small molecule drugs, and dual-target drugs pushing the boundaries of GLP-1 drug innovation, the market is expected to continue to grow.
